|
Turning Rapid Diagnostics Green — by Ailis Tweed-Kent
Outside of the laboratory at a health post in Khadi, Nepal, a throng of patients awaited the results of their rapid HIV tests. Fortunately, with recent technological advances, they would not have to wait long or travel far for the results.
Rapid, affordable, and reliable point-of-care diagnostic tests are now readily available for HIV, malaria, and syphilis in developing countries. In 2009, nearly 100 million HIV rapid tests, 70 million malaria rapid tests, and 3 million syphilis rapid tests were used for diagnosis, clinical management, case detection, and surveillance.
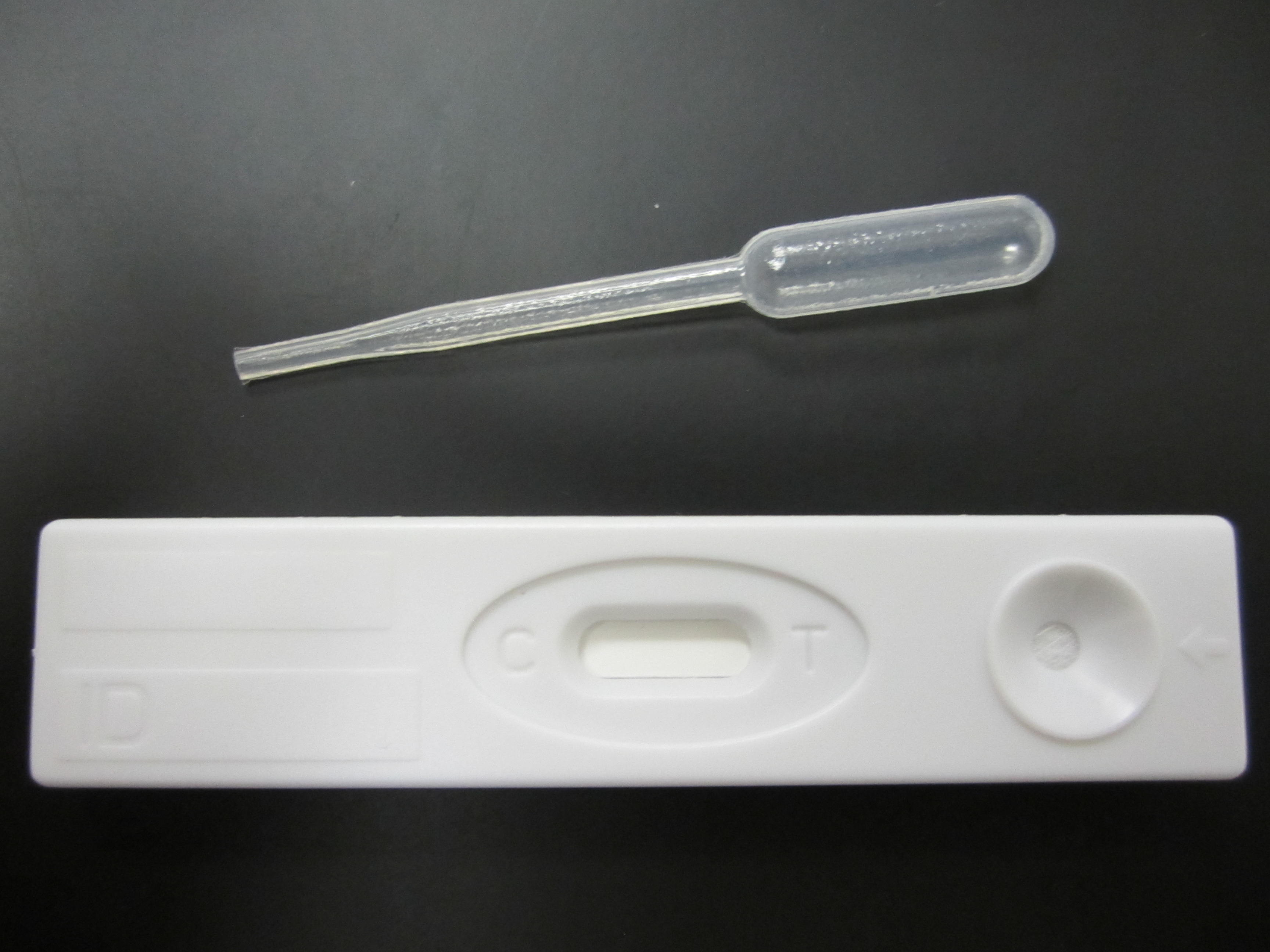
Rapid tests identify these infections by detecting antigens or antibodies in a drop of blood using lateral flow immunochromatography. Since they are intended for the point-of-care, they are designed as single-use, disposable strips made of nitrocellulose paper in a plastic cassette. Lateral flow tests like these have enabled better health care for millions of people.
In addition, a new generation of diagnostic technology has emerged that may have an even greater impact, in the form of microfluidic-based diagnostic tests. Microfluidic assays use fluid dynamics in minute volumes to process a specimen for sophisticated analysis at the point of care, harnessing a wide array of detection methods from PCR to immunoassays. Like lateral flow rapid tests, they are designed as single-use disposable cartridges made primarily out of plastic, along with a small, permanent instrument. It is projected that by 2020, more than 100 million microfluidic assays, or approximately 15,000 metric tons of plastic polymers, will be implemented throughout the world.
An issue of pressing environmental concern, however, is the disposal of millions of these plastic rapid diagnostic tests. Each year, 0.5 to 3 kg of medical waste is disposed of per person in developing countries. With the imminent arrival of thousands of tons of plastic polymer in the form of rapid diagnostics, this number will rise. In developing countries, most medical waste is disposed of via incineration or stored in landfills. In 2002, the World Health Organization (WHO) reported that up to 64% of health care facilities in developing countries do not have proper medical waste management systems.
With improper disposal, the waste from medical plastics, including rapid diagnostic cassettes, can release toxic by-products called furans, dioxins, and polychlorinated biphenyls (PCBs) into air and groundwater. These toxins can destroy surface vegetation, contaminate drinking water, and release greenhouse gases. Furthermore, plastic pollutants can accumulate in the food chain, potentially leading to toxic levels in breast milk, as well as cancer, impaired reproductive function, and impaired immune function.
Since PCBs, furans, and dioxins are considered carcinogens, international agencies, such as the United Nations Environment Programme, the WHO, and the Basel Convention have established limits on emission and tolerable intake. These guidelines are useful in theory, but in practice, few countries are able to improve medical waste management and achieve acceptable limits on the emission of plastic pollutants.
In recent years, advances in materials science have led to the development of thermoplastic biodegradable polymers—safer plastics. The main components of the new thermoplastic polymers are natural polymers, starch and polylactic acid, along with varying amounts of plasticizer, a benign chemical constituent that provides flexibility. The thermoplastic properties of these new polymers allow for injection molding, an important component in the manufacture of low-cost diagnostic tests.
Research institutes, including the National Research Council, Canada—Industrial Materials Institute (NRC-IMI), are now developing and producing these polymers, and organizations such as the Ecologically Friendly Diagnostics Working Group at the London School of Hygiene and Tropical Medicine (LSHTM), will be evaluating these polymers in rapid diagnostic tests under field conditions. If successful, biodegradable materials may alleviate the detrimental environmental effects associated with rapid diagnostic plastic waste in developing countries.
As Charles Holmes, Chief Medical Officer of the U.S. President’s Emergency Plan for AIDS Relief (PEPFAR), stated, “The development of eco-friendly diagnostics would be an important contributor to reducing waste management costs and environmental impacts in the countries in which we work.”
Beyond diagnostics, biodegradable materials should be evaluated in other plastic medical devices, such as syringes, intravenous tubing, and malaria bed nets. It has been reported that 250 million malaria bed nets will be distributed by the end of 2010, equating to 1000 metric tons of plastic polymer. After three years, when the insecticide wears off, the nets are generally disposed of in incinerators or landfills. Similar to diagnostics, the plastic degrades into dioxins, furans, and PCBs causing detrimental environmental and health effects.
Sir Richard Feachem, Executive Director of Global Health Sciences at the University of California San Francisco, notes, “Millions of expired long-lasting insecticide-treated bed nets (LLINs) are piling up in Africa and throughout the 99 malaria-endemic countries. These nets are preventing hundreds of thousands of malaria deaths but are also creating a waste disposal problem. The development of bio-degradable insecticide-treated nets would constitute an important breakthrough."
Rapid diagnostic tests have helped usher in a new era in global health, but they have come at a cost. Looking forward, an ecologically friendly agenda is essential to global health, and will only be achieved through leadership, commitment, and interdisciplinary collaboration.
First, we must raise awareness about the hazards associated with plastic medical waste. Second, we must support research and development of safer plastics, such as the work being done at NRC-IMI and LSHTM to fully characterize the material properties of biodegradable polymers. Third, the polymers must be tested in diagnostic platforms by working with product development engineers in industry. Fourth, once new materials are well characterized and tested, the economic incentives (whether positive or negative) for suppliers to switch to biodegradable polymers must be defined and outlined. This may require policy makers or governmental organizations to develop tariffs and penalties or to provide subsidies and tax credits. Lastly, biodegradable polymers should be tested in malaria bed nets, syringes, and other plastic medical devices, beyond rapid tests.
The development of biodegradable rapid diagnostic tests will require continued engagement from the global health diagnostics community, from researchers to industry to end users. We must make certain our efforts to improve health are not at the long-term expense of human health and the local environment.
|
